Incisional & PostOp Provider hygiene during CSL post surgical treatments


In recent years, the Body Altering Aesthetics industry has undergone a transformative journey toward adopting enhanced hygiene standards in line with the rigorous requirements set by the American Healthcare Standards. As the field continues to evolve and prioritize the well-being of clients, the imperative to establish and adhere to stringent hygiene protocols has become increasingly apparent. By bolstering the industry’s commitment to optimal cleanliness and safety practices, professionals can ensure the provision of top-tier care that aligns with the highest standards of healthcare. This paradigm shift toward improved hygiene measures not only elevates the overall quality of client care but also solidifies the industry’s dedication to fostering a safe and secure treatment environment for all.
Degraded infection barrier:
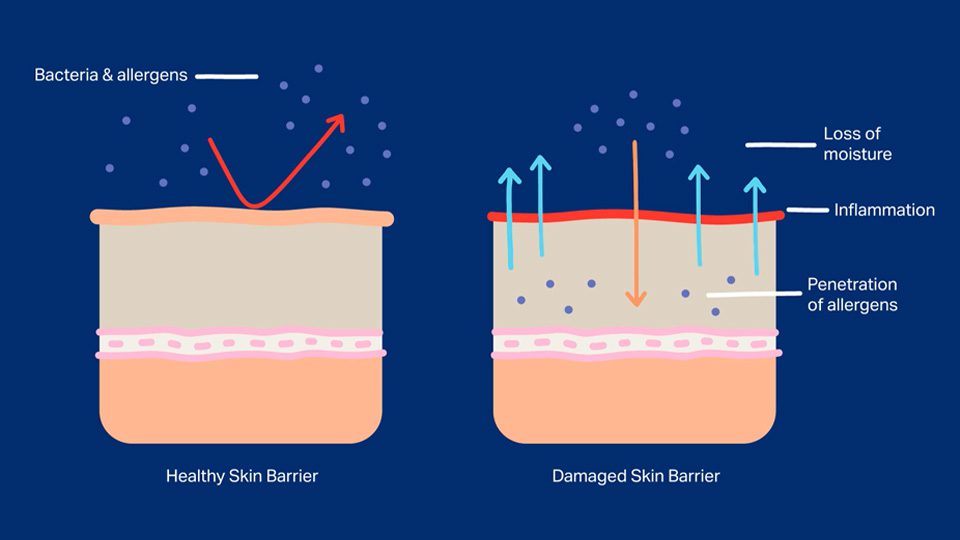
After undergoing surgical procedures, clients’ skin is rendered highly vulnerable and delicate, marked by a reduced ability to defend against potential infections due to a compromised immune system. The trauma inflicted during the surgery tends to leave the skin in a precarious state, with its natural barriers significantly impaired or disrupted. Typically acting as the first line of defense against pathogens and harmful microorganisms, the skin’s innate protective mechanisms, including its natural oils, acidic pH, and beneficial bacteria, are substantially compromised post-surgery. The disrupted skin barrier not only increases the risk of microbial infiltration and infection but also heightens the susceptibility to external irritants and allergens. Consequently, it becomes a priority for healthcare providers to exercise heightened caution and adhere to stringent hygiene protocols when dealing with post-surgical wounds and incisions.
Bacteria infiltration:
It is estimated that there can be anywhere from hundreds to thousands of bacteria per square inch on surfaces that are frequently touched or commonly exposed to human contact. These surfaces can include doorknobs, countertops, mobile phones, and other frequently handled items. The presence of bacteria is influenced by factors such as environmental conditions, human interaction, and cleaning practices.

Other examples include:
- A healthcare Provider’s watch
- Earrings or other jewelry worn by the provider
- Unsterilized or improperly sanitized gloves
- Contaminated or non-sterile equipment
- Patient’s own skin, especially if not properly cleansed before the post surgical treatment
- Airborne particles or microorganisms present in the treatment room
- Provider’s clothing, including shirt sleeves, if not adequately covered or sanitized
- Draping or linens that may have been exposed to contaminants
- Any surfaces or objects in the vicinity that may harbor bacteria, such as countertops, trays, or equipment in the treatment area; especially in domiciliary spaces.
- Surgical masks or face shields that may have accumulate contaminants during the treatment or previous treatments earlier in the day
- Hair strands
- Any personal items brought into the treatment room, such as pens, cell phones, or notebooks, that may harbor bacteria
- Floor surfaces or objects in the immediate vicinity that might not have been thoroughly sanitized
- Impure water or emollients used for cleaning or irrigation purposes during the treatment
- The bottles or containers of commonly used emollients during treatment sessions (like Ultra sound gel bottles, oil bottles, cream tubes, etc.)
- Any disposable or single-use items that have been improperly stored or handled before use
- Fabric or materials used in the treatment setting that may have retained bacteria despite attempts at sterilization
- Exposed food or drink that might be consumed without proper hand hygiene
Types of bacteria & infections:
Without proper protective equipment (PPE) and a thorough cleansing of the treatment area, several common types of bacteria may potentially attach themselves to a client’s skin after plastic surgery during postoperative massage treatments. These bacteria may include but are not limited to Staphylococcus aureus, Streptococcus pyogenes, Pseudomonas aeruginosa, Escherichia coli (E. coli), and various strains of Clostridium.
Clients who experience infections after plastic surgery due to exposure to common bacteria may develop various conditions, ranging from mild to severe. Some of these conditions include:
- Cellulitis: A common bacterial skin infection that can cause redness, swelling, and pain in the affected area.
- Methicillin-resistant Staphylococcus aureus (MRSA) infection: A type of staph infection that is resistant to several common antibiotics and can lead to severe skin and soft tissue infections, as well as potentially life-threatening conditions.
- Sepsis: A potentially life-threatening condition that occurs when the body’s response to infection causes inflammation throughout the body, leading to organ dysfunction and failure.
- Abscess formation: Pockets of pus caused by the body’s attempt to fight off the infection, which may require drainage and medical intervention.
- Necrotizing fasciitis: A serious bacterial skin infection that spreads quickly and can cause tissue death, leading to a life-threatening condition if not treated promptly.
- Erysipelas: A type of skin infection that typically affects the legs, face, or arms and is characterized by redness, swelling, and pain.
- Bacterial pneumonia: An infection that inflames the air sacs in one or both lungs, leading to coughing, difficulty breathing, and other respiratory symptoms.
- Wound dehiscence: A surgical complication where a wound reopens along the surgical incision, potentially leading to the exposure of deeper tissues and an increased risk of infection.
- Osteomyelitis: An infection of the bone that can result from the spread of bacteria through the bloodstream or from nearby tissue, causing bone pain and tenderness, as well as general signs of infection.
Tips for CSL Therapy provider Treatment compliance:
The American Standards for postoperative treatment providers to adhere to in the Body Altering Aesthetics industry for maintaining optimal treatment hygiene:

Clients:
- Creating a designated space for clients to leave their personal belongings upon entering the treatment room
- Ensuring thorough skin disinfection and cleansing before and after each treatment session; using an astringent specifically made for plastic surgery clients will allow providers to cleanse the canvas before the actual treatment application.
- Providing clients with fresh disposable linens for use during the massage to prevent cross-contamination.
- Using sterile draping techniques and materials to cover any incisions or wounds during the massage session.
- Educating clients on proper wound care and hygiene practices to follow at home post-treatment.
Providers:

- Wearing appropriate personal protective equipment (PPE) such as disposable gloves, masks, and PPE gowns during client interactions— especially the first 2 weeks after surgery.
- Wearing short sleeved scrubs; sleeves shouldn’t be anywhere near gloves as it allows for the transmission of bacteria.
- Removing watches & rings that could pierce gloves.
- Hair should be pulled back and held in place, even if short.
- Practicing proper hand hygiene by washing hands thoroughly before and after each client session and using hand sanitizers as needed.
- Adhering to strict sterilization protocols for all treatment equipment and tools, including regular cleaning and disinfection.
For the Treatment Room:

- Properly converting any non healthcare/medical domiciliary space into a hygienically sound environment
- Use appropriate barriers.
- Maintain biohazard protocols for cleaning and disposing of soiled linens.
- Maintaining a clean and sterile treatment environment, including regularly disinfecting all surfaces, equipment, and furniture.
- Ensuring well functioning ventilation within the treatment room to minimize the spread of airborne contaminants.
- Using disposable or easily sanitized materials such as paper sheets and towels, as well as single-use massage supplies wherever possible.
- Implementing a strict policy of regular deep cleaning and disinfection of the treatment room, particularly after each client session.
Conclusion
In the realm of Incisional & PostOp Provider hygiene during CSL post-surgical treatments, maintaining the highest standards of care and stringent hygiene protocols is essential. Given the vulnerability of clients’ skin after surgery and the potential risks associated with bacterial infiltration, the implementation of comprehensive hygiene measures becomes paramount. Educating both clients and providers on the best practices within the Body Altering Aesthetics (BAA) industry is a mainstay of CSL Therapy for minimizing the risk of postoperative infections and ensuring optimal treatment outcomes. Adhering to the American Standards for postoperative treatment providers, encompassing guidelines for clients, providers, and treatment room maintenance, is key to elevating the quality of care and safety measures in the BAA Industry.
This article is apart of an advisory collection that serves as a critical reference point for esteemed entities, including policymakers, health departments, and Boards of Physicians, in their pursuit of formulating and establishing American Healthcare Standards. Upholding the highest echelons of quality healthcare and adhering to the most stringent medical principles, this blog aims to contribute to the overarching framework of best practices and guidelines within the healthcare industry. By emphasizing the importance of maintaining exemplary hygiene standards, respecting legal regulations, and honoring professional boundaries, this collection advocates for a healthcare landscape that prioritizes patient safety and well-being above all else. It is with this unwavering commitment to excellence that we aim to guide and inform the decisions of healthcare stakeholders and policymakers, ensuring that every individual receives the utmost care and attention in their medical journey.
