Massaging Over Open Wounds

In the realm of postoperative care, the significance of adhering to stringent hygiene measures cannot be overstated. When it comes to the practice of Incisional Sciences and/or PostOp-Indur manual manipulation treatments over open wounds and compromised skin without prior sanitization of the client’s body, the ramifications can be severe. Not only does this approach increase the risk of introducing infections and bacteria into vulnerable areas, but it also poses a direct threat to the client’s overall well-being.

The open nature of wounds and the compromised state of the skin render it highly susceptible to harmful pathogens. Normally, the skin serves as the first line of defense, equipped with various protective mechanisms to repel external aggressors. These include the skin’s acidic pH, which inhibits the growth of harmful bacteria, as well as beneficial bacteria that compete with pathogenic microorganisms for space and resources. Additionally, the skin’s natural oils create a protective barrier that prevents the penetration of harmful substances. The epidermis and dermis work in tandem to prevent water loss, maintain the skin’s hydration, and act as a physical barrier against the invasion of microbes. However, when the skin’s integrity is compromised, these protective functions are significantly weakened, rendering the body more susceptible to infections and external irritants.
Weakened skin barriers:
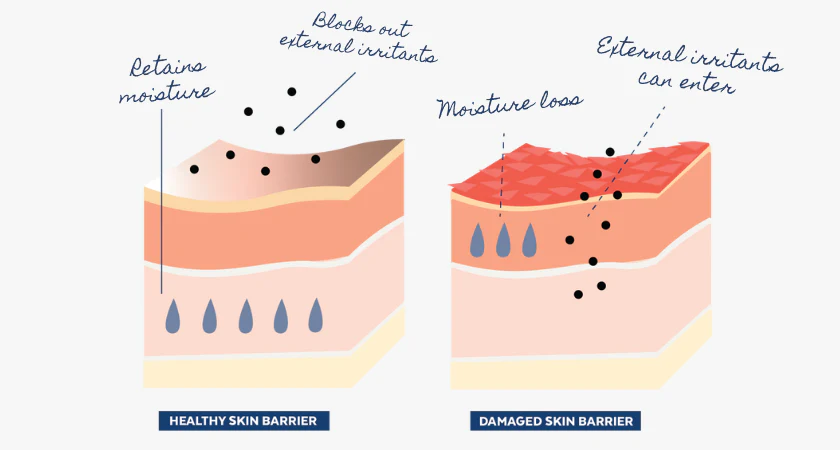
During the trauma of plastic surgery, the skin’s natural barrier, comprised of the epidermis and dermis, undergoes significant disruption at the cellular level. The integrity of the stratum corneum, the outermost layer of the epidermis acting as the primary protective shield against external aggressors, is compromised. This disruption often involves the disturbance of the lipid barrier, a major component responsible for maintaining the skin’s hydration and serving as a protective barrier against water loss and microbial invasion. Additionally, the trauma may cause damage to the skin’s microbiome, which is composed of a delicate balance of microorganisms acting as a protective shield against harmful pathogens. As a consequence, the client’s skin is left more susceptible to invasive microorganisms and external irritants, amplifying the risk of infection and hindering the natural wound healing process.
Cross contamination:
With a weakened skin barrier and a compromised immune system, the body’s natural defense mechanisms are significantly impaired, leaving the client vulnerable to potential infections. When bacteria is introduced to the skin, particularly during postoperative massage treatments, the body’s normal protective responses are hindered, heightening the risk of contamination and further complicating the healing process.

As healthcare providers navigate their hands over the client’s skin, any interaction with compromised areas such as surgical incisions or burns from surgical garments introduces bacteria to these vulnerable sites, increasing the likelihood of infection and other associated complications.
Preventing cross contamination:
In order to avoid introducing bacteria to compromised areas of the skin during postoperative massages, healthcare providers must adhere to rigorous hygiene protocols.
This includes—
- Consistently wearing disposable gloves during all client interactions and changing them whenever necessary to prevent the spread of contaminants.
- Additionally, implementing the use of astringents to thoroughly cleanse the client’s entire torso before initiating the treatment reduces the risk of bacterial transmission.
- Any expelled fluid from wounds or incisions should be handled with extreme care, ensuring that it does sit on or remain stagnate with the client’s skin or any other surfaces.

- Providers should maintain a sterile treatment environment by regularly disinfecting all equipment and surfaces, and they should use disposable or easily sanitized materials whenever possible.
- Furthermore, it is important to educate clients about proper postoperative wound care and hygiene practices to facilitate their active participation in the healing process.
Proper hygiene isn’t just a client’s right during quality treatments, it’s the American Standards within the laws of healthcare.
This article is apart of an advisory collection that serves as a critical reference point for esteemed entities, including policymakers, health departments, and Boards of Physicians, in their pursuit of formulating and establishing American Healthcare Standards. Upholding the highest echelons of quality healthcare and adhering to the most stringent medical principles, this blog aims to contribute to the overarching framework of best practices and guidelines within the healthcare industry. By emphasizing the importance of maintaining exemplary hygiene standards, respecting legal regulations, and honoring professional boundaries, this collection advocates for a healthcare landscape that prioritizes patient safety and well-being above all else. It is with this unwavering commitment to excellence that we aim to guide and inform the decisions of healthcare stakeholders and policymakers, ensuring that every individual receives the utmost care and attention in their medical journey.