Unveiling T-Interstitial Fluid: The Dynamic Fluidity of Surgical Interstitium
The intricate dynamics of bodily fluids have unveiled a novel entity known as T-interstitial fluid. This specialized fluid, distinguished by the infusion of “tumescent fluid,” presents a unique composition and behavior within the interstitium in the postoperative healing process & the body’s response to surgical trauma. Understanding the distinct characteristics and movement of T-interstitial fluid is key to comprehending the intricacies of post-surgical recovery and optimizing the management of fluid dynamics within the body’s intricate network.
Objectives of this article:
- Explore the composition of T-interstitial fluid and the role of tumescent fluid in postoperative healing dynamics.
- Investigate the movement of T-interstitial fluid through interstitial spaces, emphasizing challenges in its clearance and the impact on compromised lymphatic structures.
- Analyze the effects of heightened viscosity on internal vascular structures and lymphatic valves, highlighting the need for comprehensive understanding in postoperative care.
- Propose specialized postoperative treatments to facilitate the efficient removal of inflammatory mediators and trapped T-interstitial fluid, thereby enhancing postoperative outcomes and patient well-being.
Characteristics and Components of T-Interstitial Fluid:
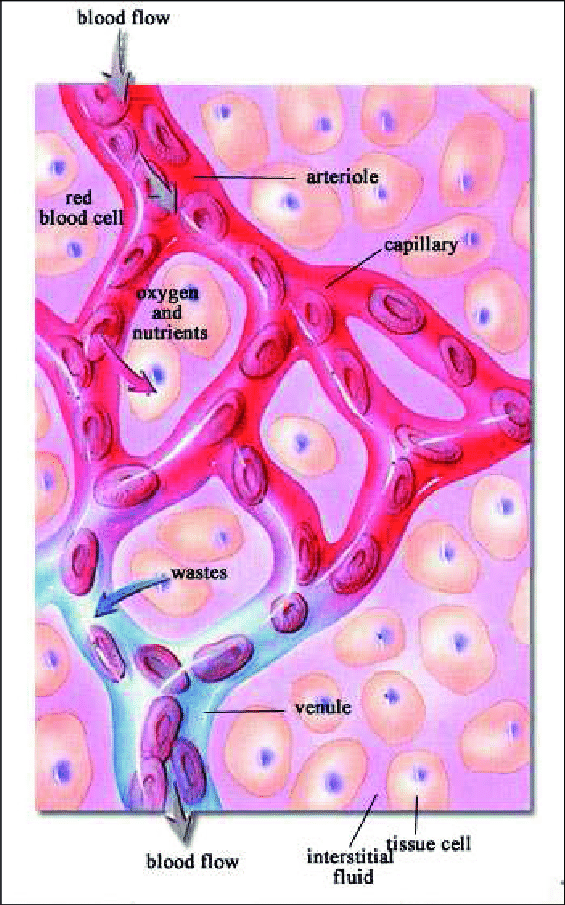
T-interstitial fluid, akin to conventional interstitial fluid, encompasses a dynamic amalgamation of water, ions, proteins, and cellular components, with the distinguishing addition of tumescent fluid. This infusion of tumescent fluid, comprising local anesthetics, vasoconstrictors, and saline, endows T-interstitial fluid with a distinctive viscosity, allowing for prolonged anesthesia, reduced bleeding, and enhanced visualization of surgical sites during procedures. Within this fluid, immune cells, including macrophages, neutrophils, and lymphocytes, stand as the vanguards of the body’s defense, initiating the intricate cascade of cellular interactions needed for expedited wound healing and tissue regeneration. Other constituents such as electrolytes and growth factors contribute to the orchestration of the inflammatory response and the stimulation of angiogenesis, fostering a microenvironment conducive to robust and rapid tissue repair.
Movement and Clearance Through the Interstitium:
Following its introduction into the interstitial spaces, T-interstitial fluid embarks on a complex journey, traversing the intricate matrix of the interstitium while enlisting the support of lymphatic structures. Navigating through the mesh-like network of the interstitium, T-interstitial fluid encounters a series of lymphangions, the functional units of lymphatic vessels, which employ a peristaltic motion to propel the fluid toward the lymph nodes and ultimately the lymphatic system. In a perfect world, everything flows fine.
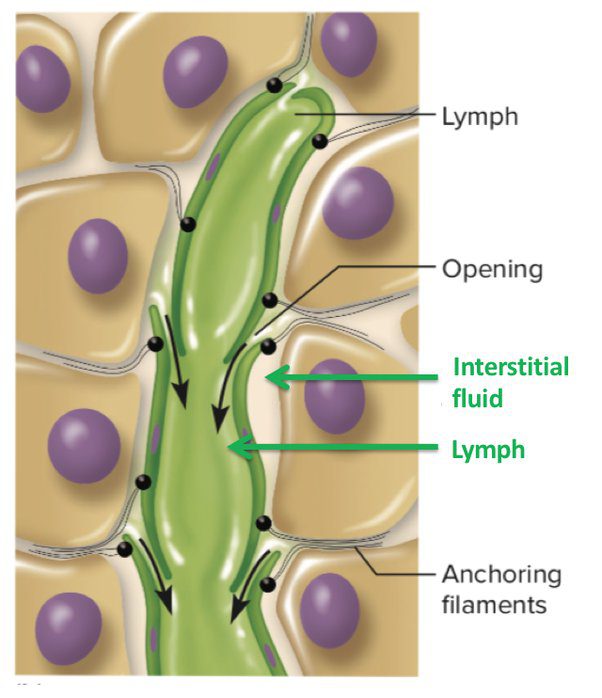
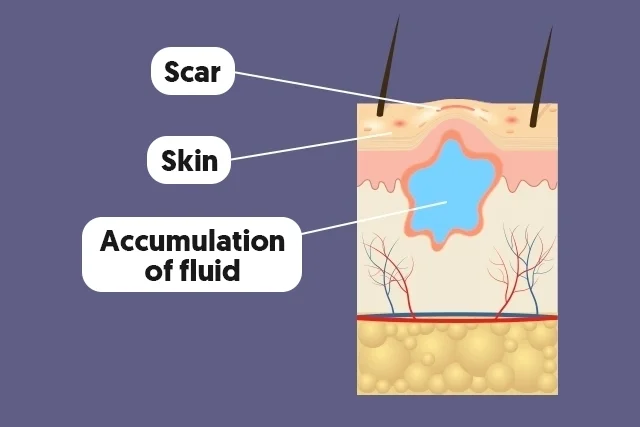
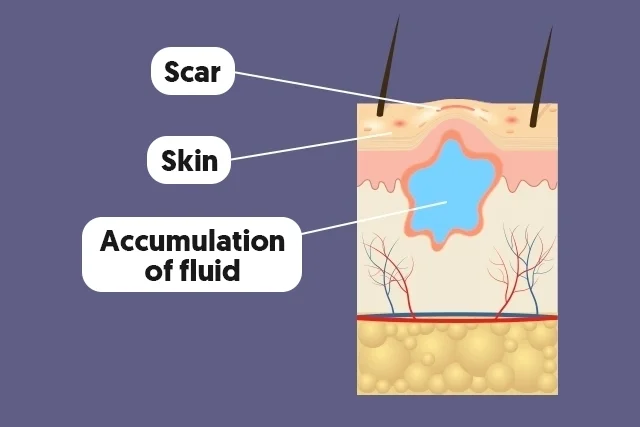
However, during most plastic surgery procedures, a lot of internal lymphatic vasculature is damaged and takes 2-3 months to rebuild. During this time, the compromised lymphatic system struggles to efficiently manage the heightened volume and viscosity of t-interstitial fluid, leading to potential lymphatic stasis and the formation of seromas, which are localized accumulations of fluid. In the absence of optimal lymphatic function, the trapped fluid may create an environment conducive to the formation of seromas, hindering the natural drainage process and prolonging the client’s recovery. Additionally, the increased pressure exerted by the trapped fluid can impede the regeneration of lymphatic vessels, further exacerbating the challenges associated with fluid clearance and extending the timeframe required for complete resolution. As the lymphatic vasculature gradually rebuilds over the course of several months, the drainage of trapped t-interstitial fluid improves, facilitating the restoration of lymphatic flow and the mitigation of postoperative complications.
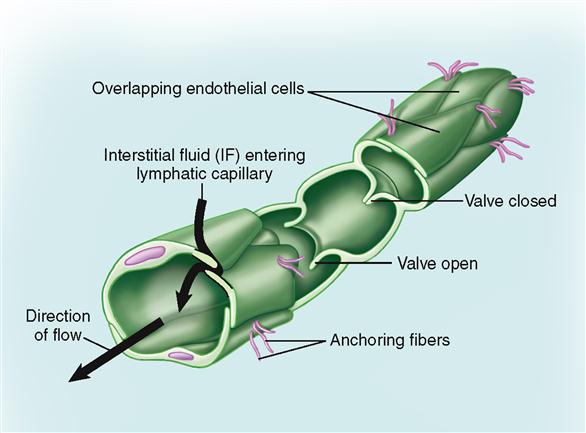
The heightened viscosity of T-interstitial fluid places additional pressure on lymphatic valves, necessitating an external/manual coordinated and efficient clearance process to maintain fluid balance. Traditional manual lymphatic drainage massage when studied and approved for lymphatic drainage, did not have the inclusion of tumescent or T-interstitial fluid.
While normally self-regulated, the trauma riddled lymphatic system’s movements are manually supported through specialized postoperative treatments + post surgical medical garments to not only facilitate the removal of metabolic waste and inflammatory mediators, but also enables the transportation of immune cells, essential for orchestrating the interplay of the inflammatory cascade and tissue regeneration. In cases where the persistence of open orifices, such as incisional wounds, allows for the egress of T-interstitial fluid, this natural drainage mechanism facilitates the body’s innate cleansing and regenerative processes.
Discerning the unique properties, cellular interactions, and trajectory of this fluid, healthcare professionals can foster a comprehensive approach to optimizing post-surgical care, mitigating complications, and facilitating the restoration of physiological equilibrium. Through continued research and exploration, the realm of T-interstitial fluid stands poised to unravel further insights, paving the way for enhanced postoperative outcomes and patient well-being.
